Introduction:Senescence is one of the hallmarks of aging and age-related conditions, including but not limited to, inflammaging, frailty, and various age-related diseases. It has been well-established that radiation and chemotherapy can accelerate senescence. While myeloablative conditioning-based allogeneic hematopoietic cell transplant (HCT) is a curative treatment for patients with leukemia. The dose of total body irradiation (TBI) conditioning has to be reduced in older patients to reduce potential high treatment-related mortality, which may still cause accelerated senescence in aged individuals, resulting in poor survival outcomes. We initiated the testing of a novel total marrow irradiation (TMI) based myeloablative conditioning in older patients to enhance the anti-leukemia effect and overall survival. We hypothesize that this new radiation preconditioning strategy may also reduce radiation-induced senescence in aged individuals compared to TBI to reduce treatment-associated side effects and improve the outcomes of allogeneic HCT. We tested this hypothesis in the present study and further investigated the mechanisms of the effects of TMI-based myeloablative and dose-escalated bone marrow transplantation (BMT) on old mice by examining the changes in expression of various senescence markers and senescence-associated secretory phenotype (SASP) in the bone marrow (BM) and selected organs.
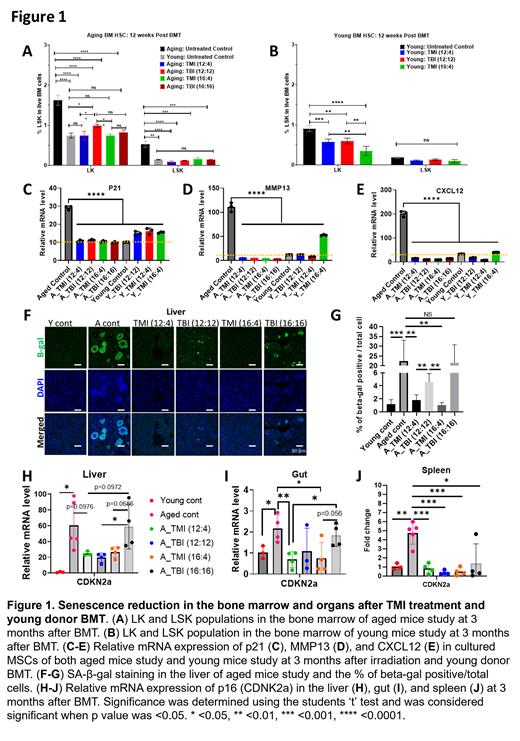
Method: The radiation treatment regimens were: TMI (12:4), TMI (16:4) and TBI (12:12), and TBI (16:16), were developed as described (Zuro et al., 2021); i.e. (12:4) means the radiation dose to the BM was 12 Gy and the dose to the organs was 4 Gy. The young (8 weeks old) and aged mice (90 weeks old) of host C57BL/6j (JAX000664, CD45.2) were irradiated in 2 fractions 24h apart, and 25 million whole BM cells from donor (JAX002014, CD45.1) were transplanted by i.v. at 24 h after irradiation. For the hematopoietic stem and progenitor cell (HSPC) population study, more mature hematopoietic progenitors (Lin − Sca-1 −c-Kit + or LK cells) and HSPCs (Lin − Sca-1 + c-Kit + or LSK cells) were examined in BM by flow analysis. Cultured bone marrow mesenchymal stem cells (MSCs) were analyzed for the gene expression of the senescence marker CDNK1a (or p21) and SASP factors MMP13 and CXCL12 by qPCR. For senescence study in organs such as the liver, gut, and spleen, senescence-associated beta-galactosidase (SA-β-gal) staining was performed and expression of the CDNK2a (or p16) was analyzed by qPCR.
Results: TMI or TBI treatment with young donor BMT repopulated the BM HSPC population without significant bone damage in aged mice (data not shown). While the BM LK and LSK populations significantly reduced in aged mice after TMI or TBI with young donor BMT compared to aged control mice ( Fig 1A), these populations were not different from young mice groups ( Fig 1B). In addition, TMI or TBI treatment with young donor BMT reduced MSC senescence. Cultured MSCs analysis showed the reduction of p21, MMP13, and CXCL12 expression ( Fig 1C-E) after TMI or TBI with young donor BMT in aged compared to aged control without radiation and BMT. However, while TMI treatment and BMT reduced senescence in the organs, mice receiving TBI treatment and BMT showed a higher senescence burden. In the liver, the aged control mice showed a significant increase in SA-β-gal staining, which was decreased in TMI (12:4) and TMI (16:4) mice ( Fig 1F). In contrast, this effect was not observed in aged mice after TBI (12:12) or (16:16) ( Fig 1G). Moreover, the senescence marker p16 expression in the liver and gut was reduced only in TMI (12:4) and TMI (16:4), not in TBI (12:12) or (16:16) ( Fig 1H, I), whereas the p16 expression in the hematopoietic tissue, spleen was decreased in all treatment groups TMI vs. TBI ( Fig 1J).
Conclusion: TMI-based dose escalates with young donor BMT in aged mice preserved BM microenvironment and reduced senescence of organs while TBI treatment causes senescence of the organs. Young donor BMT, which combined with TMI or TBI treatment, preserved bone structure and reduced senescence of HSPC and MSC. However, TMI treatment decreased the SA-β-gal staining and p16 expression significantly in organs such as the liver and gut, but not by TBI treatment. This study showed the senescence reduction in both bone marrow and organs after young donor BMT and TMI treatment. For further study, we have a plan to study the mechanism and signaling pathway of senescence reduction.
Disclosures
Zhou:Dialect Therapeutics: Current equity holder in private company, Other: Co-founder of and have equity in Dialectic Therapeutics, which develops BCL-XL and BCL-2 PROTACs to treat cancer. Member of Board of Director., Patents & Royalties: Inventor of patent applications for use of BCL-XL and BCL-2 PROTACs as senolytic and antitumor agents.. Al Malki:Tscan: Consultancy.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal